#3DStartup: OsseoLabs’ AI-Led Surgical Intelligence Platform and Material

3D printed implants have already demonstrated huge potential in the surgical space. These implants are customized for patients, can reduce operating times by hours, and improve overall operational success. Today, we’re featuring a company entering that space: OsseoLabs. A finalist for the Formnext 2025 Startup Award, the young company has two integrated core technologies: OsseoVision™, an AI-led surgical intelligence platform, and a proprietary bioresorbable magnesium (Mg) 3D-printing platform. These platforms allow for a high degree of personalization, biological performance, and cost efficiency that outpaces conventional implants by a mile. We interviewed Vikram Ahuja, co-founder and CEO of the company, to learn about how its technology works and how it impacts patients’ lives.
3DN: Could you introduce yourself and share what led you into 3D printing and co-founding OsseoLabs?
I’m Vikram Ahuja (Vicky), co-founder and CEO of OsseoLabs. My background spans engineering, business economics, and company building across EV, AI, and MedTech. Prior to OsseoLabs, I co-founded multiple venture-backed startups, including Edison Motors, which was acquired by a Singapore-listed company, giving me firsthand experience scaling deep-tech products from R&D through commercialization and exit.

Vikram Ahuja
I was drawn to 3D printing not as a manufacturing novelty, but as a systems-level solution to structural inefficiencies in healthcare—specifically the mismatch between standardized implants and highly variable human anatomy. OsseoLabs was co-founded with Patcharapit Promoppatum (Joe), a mechanical engineer and academic specializing in additive manufacturing, biomechanics, and topology optimization. Our partnership combines execution-driven company building with deep technical and clinical engineering expertise.
OsseoLabs was founded to address a clear gap in maxillofacial and orthopedic surgery, where outcomes are often constrained by off-the-shelf devices, long planning cycles, and intraoperative guesswork. We saw an opportunity to re-architect the entire workflow—from imaging, through AI-driven surgical planning, to patient-specific manufacturing—within a single, regulatory-ready platform.
Our mission is to make complex surgeries more predictable, faster, and more cost-effective by replacing generic hardware with engineered, patient-specific solutions—while advancing personalized bioresorbable magnesium implants that provide mechanical support only when clinically needed and safely resorb as healing occurs.
We are building a full-stack surgical technology company that integrates software, materials science, biomechanics, and additive manufacturing to redefine how surgery is planned, executed, and scaled globally.
3DN: Could you tell us about the technologies and materials OsseoLabs utilizes?
OsseoLabs’ technology stack is built around two tightly integrated core technologies: OsseoVision™, our AI-led surgical intelligence platform, and our proprietary bioresorbable magnesium (Mg) 3D-printing platform. Together, they enable a level of personalization, biological performance, and cost efficiency that is not achievable with conventional implants.

OsseoVision is designed to simplify the workflow of surgical planning.
OsseoVision™ is the foundation of our digital workflow. It combines AI-driven CT segmentation, automated surgical planning, topology optimization, and implant generation into a single system. This includes our patented two-step topology optimization framework, which separates external anatomical fit from internal biomechanical performance, and integrates OsseoMatrix™—our TPMS porous architecture—for controlled stiffness, permeability, and load transfer. In practice, OsseoVision™ reduces design and planning time by over 90%, improves geometric and biomechanical accuracy, and materially shortens operating room time. For surgeons, this means predictable execution and fewer intraoperative decisions. For hospitals and payers, it translates into lower procedure time, fewer complications, and reduced total episode cost.
The second core technology is our bioresorbable Mg-alloy 3D-printing platform, enabled by a proprietary laser pulsation technique and model-driven degradation control. Magnesium offers bone-like mechanical properties and naturally resorbs after healing, eliminating the need for implant removal. Historically, Mg has been difficult to print due to its low melting point and instability. Our laser pulsation process stabilizes the melt pool, ensures consistent fusion, and allows precise control over microstructure. Combined with OsseoMatrix™ and OsseoOptimized™ degradation modeling, we can tune mechanical support and resorption timelines to match bone healing across indications.

Mandible reconstruction mesh-based plate
For patients, this means better integration and no secondary removal surgery. For surgeons, regenerative fixation with predictable biomechanics. For payers, lower long-term costs driven by fewer revisions and faster recovery.
3DN: How does OsseoLabs’ technology translate into improved patient outcomes or surgical experiences?
Our technology delivers measurable improvements across clinical, operational, and economic dimensions by combining AI-led surgical planning with next-generation bioresorbable implants.
At the patient level, personalization improves anatomical fit, load distribution, and biological integration. OsseoMatrix™ TPMS architectures promote superior bone ingrowth and reduce stress shielding, while bioresorbable magnesium implants provide mechanical support only during the critical healing phase and then safely resorb. This eliminates the long-term presence of permanent hardware, reduces implant-related complications, and removes the need for secondary removal surgeries—supporting faster recovery and lower revision risk.

Talus reconstruction
For surgeons, the biggest change is confidence before entering the operating room. OsseoVision™ allows them to plan the procedure digitally, review fixation strategies, and confirm implant positioning ahead of time. As a result, there’s less trial-and-error during surgery, fewer intraoperative adjustments, and shorter operating times—often by 30–50% in complex cases. Just as importantly, it reduces cognitive load, especially in reconstructions where small decisions can have large downstream effects.
At the health system level, these benefits add up. Faster planning, shorter procedures, fewer complications, and fewer revision or removal surgeries all translate into lower total costs per case. For payers and public health systems, this isn’t just about savings—it’s about making advanced reconstructive care scalable and accessible.
Ultimately, we’re not changing how surgeons think about surgery. We’re giving them better tools and better materials, so outcomes depend less on improvisation and more on preparation and engineering. By shifting surgery from artisanal execution to engineered precision and material innovation, we enable outcomes that are more consistent, scalable, and economically sustainable.
3DN: What does a typical patient case look like?
A typical OsseoLabs case runs on a digital-first workflow that tightly integrates AI-driven planning with patient-specific manufacturing. It begins with a high-resolution CT or CBCT scan from the hospital. Once uploaded to OsseoVision™, AI-based segmentation and anatomical reconstruction are completed within an hour, giving surgeons an accurate 3D representation of the patient’s anatomy early in the process.
Surgical planning and device design usually take 1–2 days, depending on complexity. During this stage, OsseoVision™ automates much of the implant and guide generation—including fixation strategy, topology optimization, and porous structure integration—while allowing surgeons and our engineers to collaborate directly on final decisions.
Once the plan is approved, production moves immediately. Polymer guides can be delivered within 24–48 hours. Metal implants, whether titanium or bioresorbable magnesium, typically require 3–7 days for printing, post-processing, and quality assurance. All devices go through dimensional checks and validation under ISO 13485 workflows.
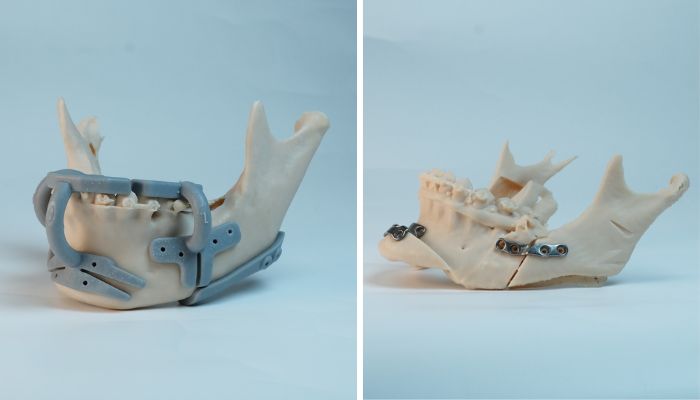
Genioplasty surgical guide (left) and genioplasty fixation plate (right)
End to end, most cases are completed within 5–10 days, significantly faster than traditional custom implant pathways. This speed is especially important in trauma, oncology, and revision surgeries, where delays directly affect clinical outcomes.
3DN: What are some of the challenges you face in developing and producing patient-specific implants?
The core challenge in patient-specific surgery is variability—every anatomy, loading condition, and clinical indication is different. That variability makes scale, reproducibility, and regulatory compliance difficult if approached with traditional device logic. Our approach has been to standardize the platform and process, rather than the implant itself, so customization does not come at the expense of control.
On the technical side, producing complex porous structures—especially in bioresorbable magnesium, a material that has historically been considered impractical for additive manufacturing—introduces an additional layer of complexity. Magnesium’s low melting point, high reactivity, and sensitivity to process instability make consistent printing, mechanical integrity, and degradation control non-trivial. We have spent significant effort solving these problems through AI-driven design rules, topology optimization, and tightly controlled additive manufacturing processes, including proprietary laser pulsation techniques and model-based degradation tuning. As a result, we have established a reproducible, ISO-ready technological foundation that can now be extended across multiple anatomical indications and use cases.
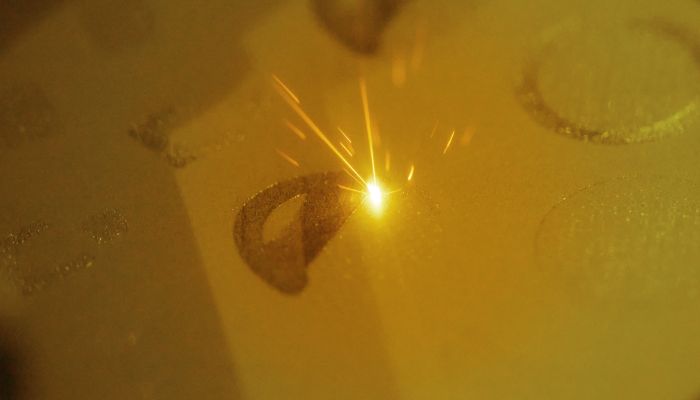
The metal printing process
Regulatory complexity is another major barrier. Personalized devices sit at the intersection of customization and compliance. We’ve embedded ISO 13485 systems, design history documentation, and risk management directly into our workflow so personalization does not introduce regulatory fragility.
Operationally, slow iteration between surgeons and engineers can stall cases. OsseoVision™ removes this bottleneck by centralizing planning, design, communication, and approval in a single environment—delivering speed without sacrificing rigor.
Finally, none of this is done in isolation. We have worked closely with strategic partners, academic institutions, and clinical collaborators worldwide to build and validate this platform, and we continue to actively welcome new partners as we expand magnesium-based solutions into broader clinical indications
3DN: What are the long-term goals or areas of innovation you’re most excited about for OsseoLabs?
Our long-term goal at OsseoLabs is to make patient-specific, regenerative fixation the default standard of care, rather than an exception reserved for complex cases. We are building a platform that systematically replaces permanent, standardized hardware with AI-designed, biologically aligned, and—where appropriate—bioresorbable implants, across a growing range of cranio-maxillofacial and orthopedic indications.
One major area of innovation is the expansion of our bioresorbable magnesium implant platform. Today, permanent implants lead to secondary removal surgeries in approximately 25% of routine cases, and in certain CMF, dental and trauma indications, removal is planned in up to 100% of patients. Our goal is to eliminate these secondary procedures by deploying degradation-tuned Mg implants that provide mechanical support only during healing and then safely resorb. Technically, our focus is on expanding degradation control, load-bearing capability, and indication-specific designs so magnesium fixation can be used not just in niche cases, but across mainstream CMF and orthopedic workflows.

Maxilla reconstruction plate and orbital floor
In parallel, we are advancing OsseoVision™ from a planning tool into a scalable surgical intelligence platform. To date, our AI-led workflow has been validated in 300+ clinical cases, delivering >90% reductions in design time and ~50% lower device costs across four automated surgical indications. Our next goal is to expand automation to a much broader set of CMF and orthopedic procedures, so personalized implants become cost-comparable to standard stock implants, and therefore the first option surgeons consider—not the last.
At the system level, our innovation agenda is tightly linked to economics. Shorter operating times, fewer complications, and avoided removal surgeries reduce total episode cost and free clinical capacity. In the U.S., this supports value-based care and bundled payment models. Globally—especially in Asia, the Middle East, and emerging markets—our goal is to make advanced, personalized reconstruction economically viable at scale, not just technically possible.
Ultimately, we see our AI, magnesium materials, and additive manufacturing platform following a similar trajectory to titanium 3D printing—moving from early adoption to broad clinical acceptance. Our long-term ambition is to help define the next generation of implant care that improves outcomes, lowers cost, and scales globally.
3DN: Any final thoughts for our readers?
Surgery is still largely performed with standardized tools, even though patients are anything but standard. OsseoLabs exists to close that gap. By combining AI-driven planning with advanced materials such as bioresorbable magnesium, we are shifting surgery away from intraoperative improvisation and toward engineered, pre-validated execution.
For surgeons, this translates into better preparation, clearer decision-making, and fewer surprises in the operating room. For patients, it means implants that fit more precisely, support healing biologically, and do not remain in the body longer than necessary. At the system level, fewer complications and avoided secondary procedures reduce total cost of care and free clinical capacity.

The OsseoLabs team
Importantly, we do not view this as a closed ecosystem. We have intentionally built our AI and magnesium technologies as a platform—one that can be extended into indication-specific devices and workflows. We believe meaningful progress in surgical care requires collaboration, and we actively welcome strategic partners, particularly medical device companies and clinical institutions, that see the value in this approach. By working together, we can accelerate adoption, expand clinical use cases, and ultimately improve patient outcomes at scale.
What do you think of OsseoLabs? Let us know in a comment below or on our LinkedIn or Facebook pages! Plus, don’t forget to sign up for our free weekly Newsletter to get the latest 3D printing news straight to your inbox. You can also find all our videos on our YouTube channel.
*Cover Image: Calcaneus implant. (All Photo Credits: OsseoLabs)







