Bioprinting Is Being Used to Create Eye Tissues

When it comes to the body, the parts relating to the fives senses are undoubtedly some of the most important. Eyesight, hearing, taste, touch and smell allow humans and other creatures to explore the universe around them and the sudden loss of one or more can be devastating. And one of those that is often affected is sight. From aging to diseases, many different factors can cause visual impairment with up to 14 million suffering from poor vision in the US alone. However, the diseases can be hard to correct and even harder to cure, especially considering the difficulties in procuring samples for testing. But what can we do to combat this?
Researchers at the National Eye Institute (NEI), a part of the National Institutes of Health (NIH) which is the primary federal agency of the US government for conducting and supporting medical research, have turned to bioprinting in order to create eye tissues. These will be used to advance understanding of blinding diseases, particularly degenerative retinal diseases such as age-related macular degeneration (AMD). Though of course not the first time that 3D printing has been used in the treatment of eyes, two previous examples are the creation of a 3D printed eye prosthetic or the 3D printed cornea from the University of Newcastle, it shows the continued versatility of the technology for a variety of applications in the medical field, especially for research purposes.
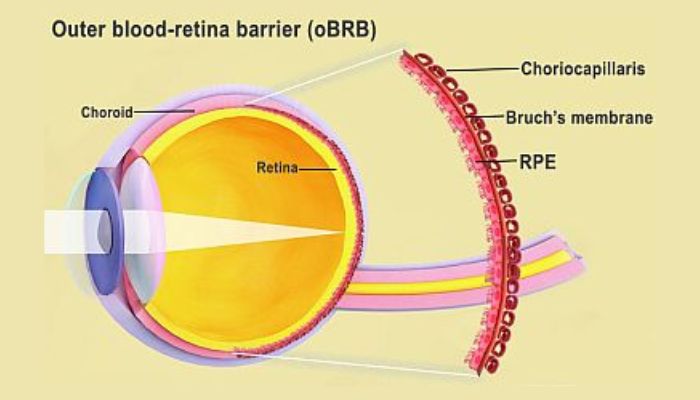
A diagram of the blood-retina barrier in the eye (photo credits: National Eye Institute)
Bioprinting Aids Research of AMD and Other Eye Diseases
Age-related macular degeneration is a common condition affecting people in their 50s and 60s. Though it does not always make patients fully blind, it essentially involves the loss of the central vision that is necessary to see details straight ahead causing blurriness and wavy areas. It is the leading cause of vision loss for older adults and nearly 20 million people in the US have some form of age-related macular degeneration, with its prevalence increasing with age. There are two forms of AMD, dry (atrophic AMD) and wet (advanced neovascular AMD) with various treatment options depending on the severity of the case. But the causes can be difficult to understand, especially the progression to advanced stages.
The NEI scientists turned to bioprinting and patient stem cells to help advance understanding of the mechanisms of blinding diseases, including AMD. They hope that the technique will provide a theoretically unlimited supply of patient-derived tissue to study degenerative retinal diseases. Kapil Bharti, Ph.D, who heads the NEI Section on Ocular and Stem Cell Translational Research, expanded “We know that AMD starts in the outer blood-retina barrier. However, mechanisms of AMD initiation and progression to advanced dry and wet stages remain poorly understood due to the lack of physiologically relevant human models. By printing cells, we’re facilitating the exchange of cellular cues that are necessary for normal outer blood-retina barrier anatomy. For example, presence of RPE cells induces gene expression changes in fibroblasts that contribute to the formation of Bruch’s membrane – something that was suggested many years ago but wasn’t proven until our model”
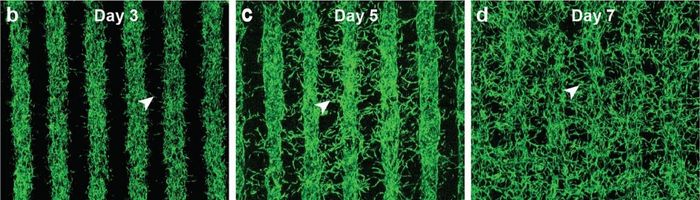
The progression of growth overtime for the cells (photo credits: Kapil Bharti)
In order to create these tissues, Bharti and his colleagues combined three immature choroidal cell types in a hydrogel. This consisted of perictyes and endothelial cells, key components of capillaries and fibroblasts to give structure. This gel was printed on a biodegradable scaffold and within days the cells had begun to mature into a dense capillary network according to a press release about the project. Indeed, the printed tissue so far seems to be viable, after reaching full maturity at 42 days. The tissue analyses and genetic and functional testing showed that the printed tissues looked and behaved similarly to native outer blood-retina barriers. Even better, under induced stress the tissue exhibited patterns of early AMD.
Right now, the researchers are uses the printed tissues to study AMD while also experimenting with adding additional cell types to the printing process to understand recapitulate native tissue even better. Co-author and director of the 3D Tissue Bioprinting Laboratory at NIH’s National center for Advancing Translational Sciences, Marc Ferrer, Ph.D., concluded “Our collaborative efforts have resulted in very relevant retina tissue models of degenerative eye diseases. Such tissue models have many potential uses in translational applications, including therapeutics development.” You can find out more in the press release HERE or in the study HERE.
What do you think of the use of bioprinting to create eye tissues? Let us know in a comment below or on our Linkedin, Facebook, and Twitter pages! Don’t forget to sign up for our free weekly Newsletter here, the latest 3D printing news straight to your inbox! You can also find all our videos on our YouTube channel.






