3D Printing Is Revolutionizing Surgical Planning, and It’s Only the Beginning

Imagine what it was like when X-Rays were first introduced. Or CT scans, and MRIs. Think about how transformative that technology was, giving physicians the ability to see inside a patient’s body without opening them up. A whole new world, right?
The same transformation happened with the advent of 3D printing for surgery. Instead of being limited to images on a screen, doctors and patients alike were allowed to use physical, 3D tools to comprehend information. Today, several hospitals regularly use the technology to visualize complex or rare cases, and the results are remarkable: operating times can be reduced by hours, surgical outcomes can be improved and patients can go into an operation with a better understanding of the situation.

Image Credit: Stratasys
And it is only the beginning—the number of hospitals in the United States with point-of-care 3D printing went from three in 2010 to over 100 today. There are so many 3D printing applications for surgery, from creating surgical guides to customized implants, and with growing interest in the field, new applications will surely develop. In this article, we are putting tools for surgical planning in the spotlight to explore how these devices are making an impact.
How 3D Printing is Used for Surgical Planning
There are various types of 3D-printed tools used for surgical planning. Below, we will highlight three of the most common ones. As this technology is still relatively new, these tools are often referred to by different names, and we will include their alternative terms for clarity.
Surgical Model
Surgical models are 1:1 scale 3D representations of a patient’s anatomy that help frame a surgeon’s approach to an operation. A step further from the traditional CT or MRI scans, surgical models are a translative tool that showcase the spatial relationship between organs, bones, or tissue—whatever anatomy is pertinent to the case. Often, surgical models are used to understand where tumors are in relation to surrounding anatomy and to develop reconstruction strategies. These are informative for the physician as well as the patient and their family.
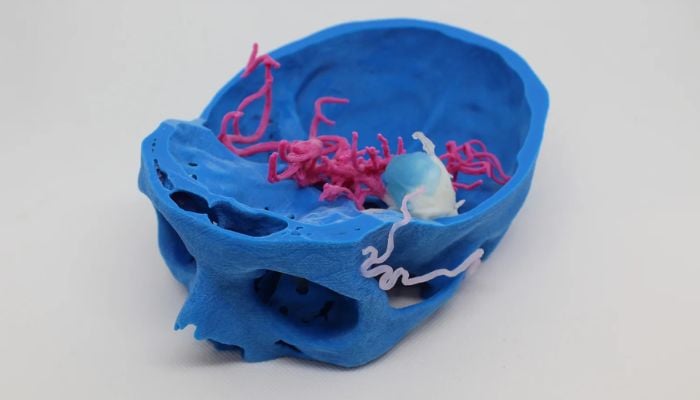
Surgical model of a 3D printed patient-specific model representing a cerebral artery aneurysm. (image credit: 3D4MED)
Surgical Guide
Also referred to as a patient-specific guide (PSG) or cutting guide, surgical guides are used to direct a surgeon during the operation. These single-use tools are custom-made for the patient and then applied directly to the body during the surgery. They function like a template, or stencil, by showing the surgeon where to put a blade, screw or whatever tools they are using. Sometimes, they can indicate the depth and direction of a maneuver. Essentially, surgical guides help ensure procedural exactness. They are used for various surgeries, common ones including craniomaxillofacial surgery, dental surgery, osteotomies and orthopedic surgery.

Patient-specific pelvic cutting guide 3D printed at Insight Surgery’s in-house manufacturing facility within Children’s Nebraska. (Image credit: Insight Surgery)
Simulation
Simulation models are similar to surgical anatomical models, but rather than being for a patient-specific case, they are used for education and training. These can be designed in the same manner as a patient-specific case, but because they are not being used for presurgical planning for a specific patient, they can be modified or even created without using Radiologic imaging. They can have lifelike characteristics where each piece of anatomy mimics the real tissue. The flesh feels like flesh, the bone feels and mimics bone, organs feel specific to each organ’s density, operating as a potential alternative to cadavers. Surgeons can perform fully simulated operations on these models. Phantoms are a specific type of simulation used in Radiology practices for training in X-ray, CT, MRI, and Ultrasound practices. In these simulations, the 3D printed materials will look very similar to real patient tissues, creating better training for the imaging professionals and resulting in lower radiation dose (or scan time for MRI/Ultrasound) for the patient.

Surgeons practicing on a 3D printed pediatric heart model (image credit: Stratasys)
Why 3D Print a Tool for Surgery?
3D printed tools are not necessary for every surgery, so what justifies their production? For surgical models and guides, the case will usually involve unique or complex anatomy—a case that is not clear with just MRI or CT scans. According to Dr. Peter Rose, an orthopedic tumor surgeon at the Mayo Clinic in Rochester, Minnesota, these cases are often in the central part of the body.
He explained, “If someone’s got a tumor around their knee, for example, it’s pretty easy to understand…and the cuts that you make for the most part are going to be fairly straight cuts that you can do with an x-ray camera to guide you and a cutting jig, or freehanded. But when we have tumors which are in and around the pelvis, for example, or tumors which are in and around the spine, where it is very complicated and spans several different anatomic compartments…[3D printing] is an extremely helpful thing to do.”
Dr Rose noted that, for cancers, it is important to remove a cancer entirely and in one piece with a cuff of normal tissue around it as a margin. “The anatomy that we need to work around oftentimes isn’t straight and rectangular,” he said. “It curves and it moves, and so [3D printing] has allowed us to identify trajectories that we would use to make a cut around things.”

Surgical model of a tumor (black and purple) on the pelvic bone (white), along with the venous (blue) and arterial (red) vessels. This patient-specific model was used to plan the surgical resection of the pelvic tumor, so the surgeon could better understand the mass’ morphology, localization and vascularization (image credit: 3D4MED)
Phantoms and simulations, on the other hand, might be printed for general surgical training or for practicing specific patient cases. Seattle Children’s Hospital, for example, 3D prints the tracheas of patients who have trouble breathing. Then, their ear, nose and throat surgeon can cut and make stitches in the 3D print, practicing surgery before the real operation.
What Is the Process Like?
For every 3D printing process, the first step is always creating the 3D model, whether it be through a scan or an imaginative design. Because taking a CT scan or MRI is already part of the pre-operative process, scans are already available for 3D printing. Using these MRI or CT scans from the radiology department, 3D imaging specialists can develop 3D models of the desired anatomy. Of course, the process for 3D printing surgical tools will look different depending on whether a hospital 3D prints themselves or outsources the prints. In this section, we will go over the general workflow for 3D printing parts in hospitals.
Once the scans are obtained, 3D imaging specialists have to do segmentation, which means defining what structures are desired for better visualization. Identifying the boundaries of various parts like tumor, bone, organs and blood vessels is the main objective of segmentation. Often, this has to be done manually for 3D printing, because the cases that are 3D printed are almost always unique. However, some AI solutions have been integrated into this process.
Children’s Nebraska’s Manager of 3D Gabe Linke explained, “In some instances, [AI] helps get us a little bit further to start, but then we have a lot of manual work… We’re excited because as AI gets better, it will probably take less and less data to train successful models.”
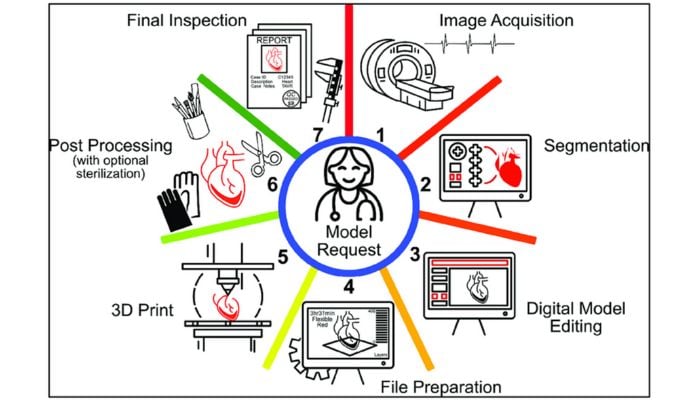
Image Credit: Bastawrous et. al.
Technologies and Materials
Once the 3D file is prepared, it is time to print—but what technologies and materials should be used? The process requires consultation with doctors and 3D imaging specialists or engineers—in any case, people who specify the case’s needs. Various kinds of 3D printing technologies are utilized for surgical planning tools.
Adam Wentworth, former Senior Engineer at the Mayo Clinic and currently Senior Product Development Engineer at Ricoh, explained that the most common 3D printing technologies used are material extrusion (FDM), vat photopolymerization (SLA) and material jetting (Polyjet). To a lesser extent, he said, powder bed fusion with nylon 12 or thermoplastic polyurethane is used too.
Depending on the case, one technology might be favorable over another. Because 3D printed surgical planning tools are all about helping people visualize a situation, some of the most important 3D print qualities that a technician considers are related to the visual effect of the piece, i.e., whether the print will be multi-color, multi-material and/or transparent. The team can also consider whether they want the piece to be able to open, revealing anatomy inside. Another aspect is the texture of the piece and whether or not it should mimic the feeling of real anatomy.
Below, look at the difference between a CT scan, a flat image with shades of gray, versus a 3D printed device: an object with high contrast colors and tangible features. It is much easier to see what is going on with a 3D print compared to a scan that is not as intelligible to those without medical backgrounds.
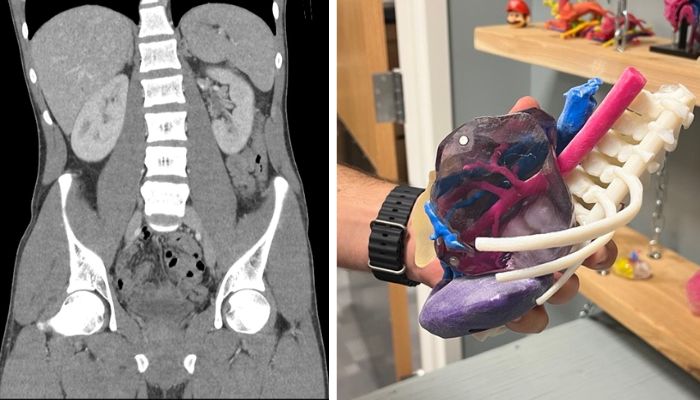
On the left, a CT scan of the abdomen and pelvis (Image credit: Mikael Häggström, M.D.), and on the right, a 3D model created for a patient at Children’s Nebraska with a complex abdominal tumor. (image credit: Julia Steiner)
Several companies, like Formlabs, EOS, Lithoz and Raise3D, produce 3D printers for medical applications. Stratasys is another that has made a name for itself as a medical 3D printer manufacturer, and we can get a sense of the desired traits for additive manufacturing in healthcare by looking at the company’s medical solutions.
The J5 MediJet, which is advertised as an all-in-one medical 3D printer, and the Digital Anatomy printer series, can produce sterilizable material, which is especially important for surgical guides that guide a surgeon’s hand. Additionally, they can print materials that react to force in the same way as human tissue or bone. This is useful for simulations, so that when they are manipulated, it mimics the feeling of operation. Additionally, the Stratasys printers can make prints with biocompatible materials, useful for implants or other objects that are in contact with the body.

On the left, a 3D print made of Stratasys’s TissueMatrix, which, soft and contractile, behaves like an organ when force is applied. On the right, a 3D print made of Stratasys’s BoneMatrix, which creates material depositing patterns mimicking porous bone structures, fibrotic tissues and ligaments. (Image credits: Stratasys)
Before Operation
After the file is printed, any post-processing will depend on the technologies used and the demands of the case. Finally, a 3D printed part will make it to the briefing before the operation.
Dr. Rose set the scene: “At the start of any operation, we have what’s called a briefing and a briefing is before the patient enters the operating room, where the lead surgeon goes through what the plan is for the case, what the anticipated needs are, what the potential pitfalls are for the case…and the 3D printed model is front and center…because it orients everybody in the operating room from the anesthesia team to the XRAY tech, to the folks that help us with implants and instruments. Everybody gets an intuitive understanding of the goals and the nature of the operation, far better than just looking at slices of a CAT scan.”
Hospitals with In-House 3D Printing Units
Several hospitals are leveraging 3D printing technology, but far fewer have in-house 3D printing. Instead, many choose to outsource their 3D printed tools. There are many companies dedicated to providing this service, including Insight Surgery and MedScan, to name a few.
Utilizing an external provider can sometimes be easier because they already have the expertise, tools and operating professionals to print the part. Additionally, external 3D printing companies could have access to technologies that would be impractical or unsafe for a hospital to have, like machines capable of metal 3D printing.
While these 3D printing providers can have strong relationships with their clients, using an external service can result in longer lead times, meaning a hospital may not receive a part for several weeks. Dr. Rose explained the dynamic. “We have had inadvertent delays happen, where we could not use an implant because of cancer progression and lead times. Companies have swallowed the cost of that, which, honestly, we didn’t need them to do…We have a good partnership with industry, but we try to do most of it in-house just because there is an inherent synergy to doing it with your own people.”

Some of the Mayo Clinic’s vat photopolymerization 3D printers (image credit: Mayo Clinic)
Minnesota’s Mayo Clinic has one of the strongest point-of-care (POC) 3D printing units in the United States, and they have been paving the way for other hospitals. With over 100 hospitals in the United States with POC 3D printing capabilities today, and the U.S. Veterans Health Administration (VHA) going from three 3D printers in 2017 to 60 in 2020, there is no sign of slowing down. According to Precedence Research, the global 3D printed surgical models market size alone is anticipated to reach around USD 2,841.23 million by 2034, expanding at a CAGR of 15.02% over the forecast period from 2024 to 2034.
The Benefits
The most meaningful effect of these surgical planning tools is that they can reduce operating times and improve operating outcomes. One systematic review published by the BioMedical Engineering OnLine, which analyzed 227 surgical papers, found that 82 percent of studies on 3D printing and preoperative planning noted better surgical outcomes when 3D printed models were employed instead of standard preoperative planning, and more than 50 percent of studies in the review demonstrated a decrease in operation duration.
That review was published in 2016, but 3D printing continues to demonstrate similar results—or even better. Ryan Cameron, Vice President of Technology and Innovation at Children’s Nebraska, said that thanks to 3D technology, “we routinely see gains between 20 and 50 percent reduction in surgical time…That’s normal for us.”
And having faster operations is not just about saving time: it also means that a patient can spend less time on anesthesia, have less intraoperative blood loss, and have a reduced need for intraoperative fluoroscopy. Furthermore, because 3D printing helps surgeons achieve greater accuracy and precision, these tools, in some cases, can reduce the need for multiple operations. As Linke explains it, simulating the surgery with 3D printing beforehand takes longer, “but it can limit the potential for repeat operations, because we had a better surgical plan going into the operation room.”

A patient-specific chest phantom created by Children’s Nebraska for simulation and training on intervention and approach for a coarctation of the aorta. (image credit: Julia Steiner)
Prior to the surgery, these 3D tools can also benefit the patients and their families. Dr. Rose said that by showing them 3D models, “we can let them be an active partner and let them decide, ‘is this surgery the right thing for me?’”
It gives Dr. Rose more peace of mind, knowing that a patient has a better understanding of their surgery. “These are incredibly difficult things that patients and their families go through,” he said, referring to his cancer patients. “And the ability for them to look at a model that they can hold in their hands helps them better understand the nature of their tumor operation.”
Essentially, these 3D tools give people clarity. Whether someone is a student practicing surgery on a simulation, a surgeon reviewing an operating plan or a patient understanding their own situation, the tools provide a clearer picture of medical scenarios, all while improving surgical outcomes.
Addressing Challenges Going Forward
Unsurprisingly, one of the challenges accompanying 3D printing surgical tools is the expense. Wentworth spoke to the current limitations: “Some AM technologies still require very experienced technicians to operate and maintain for reliable use,” he said. “As a field that is in early stages of using AM, cost for setup with industrial equipment, facilities and running cost of consumables, software and salaries can be prohibitive with unknown return on investment. Service bureaus can provide immediate access with a validated process in ISO certified facilities with slightly less favorable returns and logistics until a point of care center is built.”
However, the current challenges of creating 3D printed surgical planning tools will change as the technology continues to advance and is more widely adopted. Linke, who started the 3D printing lab at Children’s Nebraska, explained that while their hospital did not have a high barrier to entry thanks to financial support, “we just can’t hire and train enough people fast enough to keep up with the demand.” Now, the hospital is prepared for exponential growth.
As the infrastructure for 3D printing in hospitals improves, technology advances as well. Artificial intelligence, the buzzword on everyone’s mind, is already playing a role, as mentioned, in segmentation technologies. While they do not look for automation, Cameron said that, sometimes, “there’s really not an option to remove the AI,” because the technology is automatically integrated into certain software.
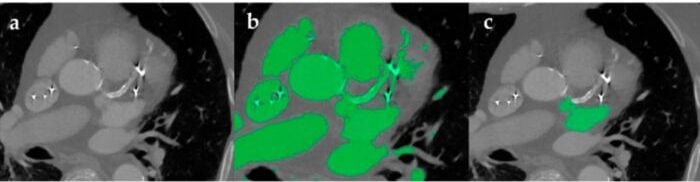
The image segmentation process of the heart with bright artifacts as a result of metal implant and arterial calcification. Part b shows automatic segmentation, which is diminished by the artifacts. Part b shows how manual segmentation was used to isolate the area of interest. (Image credit: Segaran et. al)
Yet, that does not mean they are letting artificial intelligence fully take the reins. Cameron explained, “Any decision that’s autonomously made outside of the purview of a physician or a caregiver is not something that we’re really interested in.” Instead, they focus on decision support systems, systems that can help them be more efficient, but never to make a decision. “We are very cautious and conscientious of AI products that promise software autonomy, and we’ve been intentionally avoiding that space,” Cameron added.
In addition to software improvements, printing technology has proven to continually advance, with printers achieving more life-like, multi-material prints faster and with more accuracy than ever before. As Wentworth put it, “More applications will reach later stages of maturity that warrant investment due to their published and proven impact. My vision is that these currently siloed initiatives will flourish and inspire others to pursue what is possible, though practically, reimbursement will likely be what drives adoption.”
Indeed, cost will play a major role in determining how hospitals leverage the technology. Each institution will look different, but for Children’s Nebraska, the 3D printing advancement is mostly paid for by the hospital, which they can only afford thanks to community support. “The benefits definitely outweigh the costs,” Cameron affirmed.
With all this progress, the use of 3D printed tools for surgical planning is poised to become an essential part of modern healthcare. The technology is there and improving every day—it is only a matter of finding the people and the funding to maximize impact and ensure the best care.
What do you think of using 3D printing for surgical planning? Let us know in a comment below or on our LinkedIn, Facebook, and Twitter pages! If you are looking for more 3D printing in medical & dental content, check out our dedicated page HERE. Don’t forget to sign up for our free weekly Newsletter here, the latest 3D printing news straight to your inbox! You can also find all our videos on our YouTube channel.
*Cover Image Credit: Stratasys






